Everyone inherently knows that a brain aneurysm is deadly, but what does it really mean? With the shock of the emergency behind you, we begin to read the small print to find some truly disconcerting facts that are only disclosed on an as needed basis. It’s the medical profession’s way breaking the news to you slowly. Little by little a clear picture emerges of the devastation of this type of brain injury.
The first surprise it that the brain surgery is easy part of the procedure. Opening the skull and clipping the aneurysm is low risk compared to the recovery period. How can that be I wondered? Apparently surviving a ruptured aneurysm means that you suffered an subarachnoid hemorrhage or in layman terms blood pooled in the fluid between your skull and your brain. This is a very dangerous condition since red and white blood cells can not survive in the cranial fluid and over a period of three to four days the blood cells will die. As the blood cells die and decompose they can be viewed as small sacks of toxic poisons that are released into the cranial fluid. The most critical point of recovery is four to seven days after the surgery as the toxins from decomposing blood cells reach their maximum concentration.
As these toxins build in the cranial fluid they irritate the veins carrying blood to the brain. The natural tendency of the veins is to spasm and contract. If any vein becomes excessively irritated it will spasm and completely close resulting in a loss of blood to large portions of the brain or what is called a stroke. Where the aneurysm is located, degree of bleeding and distribution of the blood inside the skull dictate your chance of survival. During the operation the surgeon will attempt to remove as much blood any possible from the injured area. While some anchoritic hemorrhages are defused deep into the recesses of the brain tissue where vascular spasms are more probably, my wife was fortunate that most of the hemorrhage was contained in the frontal lobe.
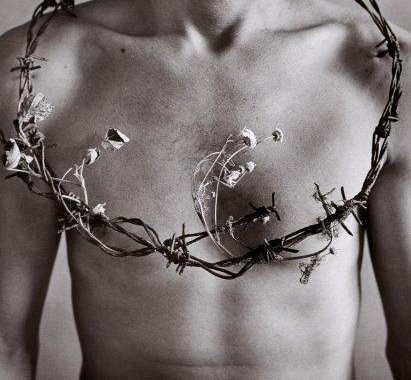
The difficult part of the recovery is the waiting knowing that each day the risk of death is on the rise until the fifth to seventh day. Each day you sit unable to help, knowing that tomorrow might be the end. Quietly you are surrounded by elaborate machines and wires staring at the numbers displayed on a computer monitor afraid to look away. You learn to read the graphs and understand the beeps and alarms. This graph is oxygen level, that graph is heart rate, that number is blood pressure. That tone is a sensor alarm, this beep means a patch has fallen off. Each movement changes the graphs as your heart jumps into your throat wondering if the erratic graphic is just a temporary disturbance or a new serious condition.
The nurses in ICU tell us take we need to watch for changes in brain function. I ask what that means, what am I looking for? A change in brain function is a sign that the patient has had a vascular spasm or a stroke. Symptoms include slurred speech, disorientation, emotional eruptions, prolonged sleep, or weakness in extremities. Besides sitting watching the monitor you observe and scrutinize the smallest of activity. Is she blinking her eyes excessively? Should she remember what day it is? Has she been sleeping too long? Your mind is hypersensitive every moment as time creeps second by second.
Slowly the person you know so well periodically emerges from the fog, but it doesn’t come without effort and loss. At first there is no memory of our pets that she has daily cared for over the past five years. There is no memory of a private joke that been told thousands of times over the past twenty years. There are moments when she stares at you and doesn’t remember that you’re her husband. She asks her mother where her mother is. While she sleeps at night and you are alone in the ICU room you begin to ask yourself difficult questions. What if she doesn’t make it back all the way? What if she can’t work and requires home care? What if she dies? Sleep doesn’t come easy at night in ICU especially since to check brain function aneurysm patients are awoken every fifteen to sixty minutes throughout the night.
You stare in amazement at the list of twenty four drugs printed in large black oversized type that hanging over her bed indicating the drugs that are being pumped into her. You are hypnotized by slow methodical drips of the rack of IV bags, but most of all you just wait. Then out of the blue, the person you know is back to normal for a few minutes. There is so much small print that we never knew.
Probably the most surreal moment is reading the surgeon’s report of the operation. In clinical precision he describes how her brain surges from the skull to relieve the pressure from the hemorrhage. How a massive blood clot that shows signs of drying is evacuated from beneath first fold of the frontal lobe. How the aneurysm is masked by a second massive blood clot deeper in the brain tissue. How the aneurysm was clipped and lanced to remove another blood clot. How the patient “tolerated the procedure”.
Finally the attending surgeon explains the small print to you in terms that you can understand while your breath is stolen. “Of the past one hundred patients that were diagnosed with a cranial aneurysm and subarachnoid hemorrhage ninety died and eight are institutionalized with severe neurological dysfunction. Only you and one other girl have survived to resume their lives.”
“The most astonishing thing about miracles is that they happen.”
G. K. Chesterton (1874 - 1936)
G. K. Chesterton (1874 - 1936)